Parathyroid Gland Function & Development
Unless you have parathyroid disease or know someone who has it, chances are that you have never heard of the parathyroid glands. The four parathyroid glands are located in the lower neck, behind the thyroid, and they are part of the endocrine hormonal system. The thyroid gland and the parathyroid glands are not related in terms of what they do; they are just next to each other. The prefix “para” means next to; since the parathyroid glands were discovered long after the thyroid and their function was not clear at the time, they were simply named the parathyroid glands based on their location, but they do not have the same function or purpose as the thyroid gland.
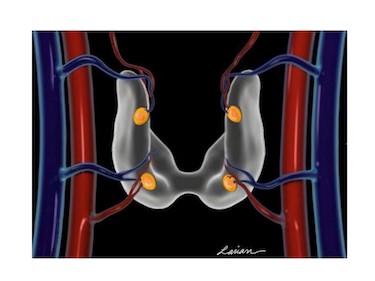
The parathyroid glands consist of two sets of small, oval-shaped glands, and a typical parathyroid gland is fairly flat and roughly about the size of a pea. The parathyroid glands are located next to the thyroid gland lobes in the neck, and they develop in humans at the same time as the thyroid gland and share the same blood vessels. The major branches of the thyroid arteries and veins go to the thyroid gland, and the very small branches go to the parathyroid glands.
Parathyroid Glands Regulate Calcium
Parathyroid glands are mainly responsible for controlling the calcium levels in the body within a very narrow range so that the body can work properly. Calcium is a vital nutrient that is used by every single cell in the body for normal daily functions; it is responsible for sending messages inside the cells, building bones, sending signals in-between nerves, flexing muscles, and so much more. If calcium levels are not exactly right, a variety of problems can happen, including bone loss, intestinal symptoms, kidney disease, and mental disturbances.
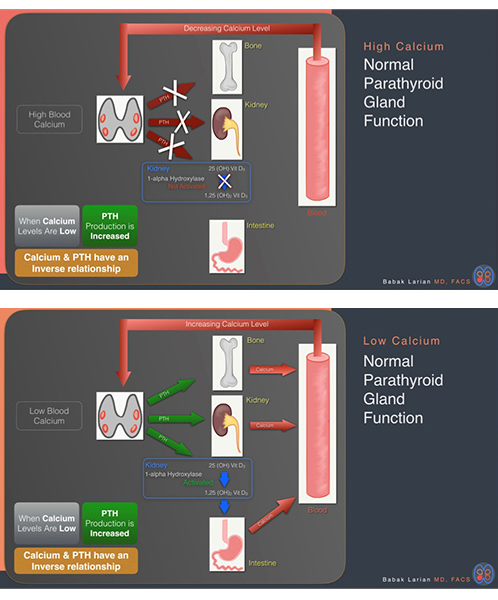
We have four parathyroid glands (when one would be enough to do the job) because maintaining precise calcium levels is so important to our body’s ability to function properly on a daily basis. To regulate calcium, the parathyroid gland controls the amount of a chemical called parathyroid hormone (PTH) that it releases into the bloodstream. Each parathyroid cell has a calcium sensor to detect the level of calcium in the blood. When calcium levels are high, the parathyroid gland “turns off,” and the body’s PTH level decreases. Alternatively, when the calcium sensor detects that calcium levels are low, the gland “turns on” and produces PTH, which pours into the bloodstream and instructs the body to put more calcium back into the blood.
The parathyroid glands measure the amount of calcium in the blood every minute of every day, and if the calcium levels are lower than the parathyroid gland wants, the glands will recognize it right away and make PTH. Next, PTH goes to other parts of the body, mainly the bones and kidneys, and instructs them to increase the calcium in the blood. When the calcium level comes up again, the parathyroid gland shuts down and stops making PTH. Through this feedback loop, the body is able to have precise control over the level of calcium in the blood.
Dr. Gordon Strewler published an interesting article in 2005 that showed the relationship between calcium and PTH. He showed that there is an inverse relationship between calcium and PTH, with PTH being low when calcium is high, and PTH high when calcium is low. The first graph below shows his results. Dr. Strewler found that when the calcium level changes only a minimal amount, the parathyroid gland responds immediately to bring the calcium back to the person’s normal (called the calcium set point). The calcium set point functions similarly to a thermostat; when you set the temperature to 70°F, the heater will work when the temperature in the house goes down to 67°F, and stop working when it goes above 70°F.
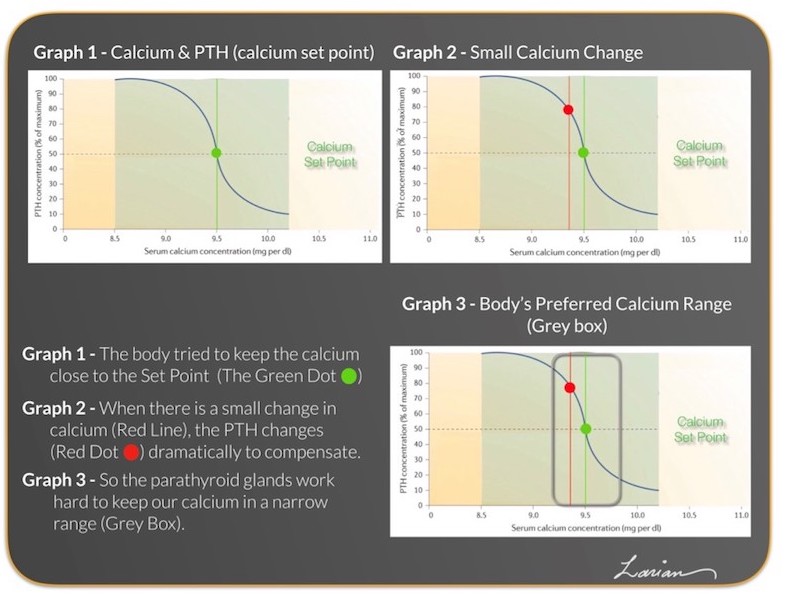

Each individual’s calcium set point is different. Some calcium set points may be in the lower ranges of the reference values (what laboratories call a normal range); for example, 8.8mg/dL. Meanwhile, some are in the middle range (9.5mg/dL), and some in the higher range (10.0mg/dL). As these graphs show, an individual’s calcium set point value does not matter, as his or her parathyroid gland ensures that the calcium level is always either maintained at a specific level or brought back to that level.
The parathyroid glands keep calcium at the calcium set point or close to it. If the set point is 9.5 mg/dL as in the graphs above, then the parathyroids will work 24 hours a day to keep the calcium level close to that. If there are slight changes, the parathyroid glands react immediately to bring the level back to the set point. The body can tolerate an elevated or reduced calcium level for a short period of time, but when an elevated or reduced level stays the same for an extended period, then all organs begin to malfunction. So, the range of normal that the parathyroid will allow is a very narrow range. As seen in Graph 3 above, the set point is 9.5 mg/dl, but the range is the area in the grey box from 9.2-9.8 mg/dl. Calcium may occasionally go out of that range, but as you can see based on the graph, the PTH reaction is dramatic to bring the calcium back into range. The laboratory normal range (also known as the reference range) is shown in the graph as the green shade (8.5-10.2 mg/dl) in between the yellow shaded areas at the two ends of the graph.

PTH and PTH Receptor
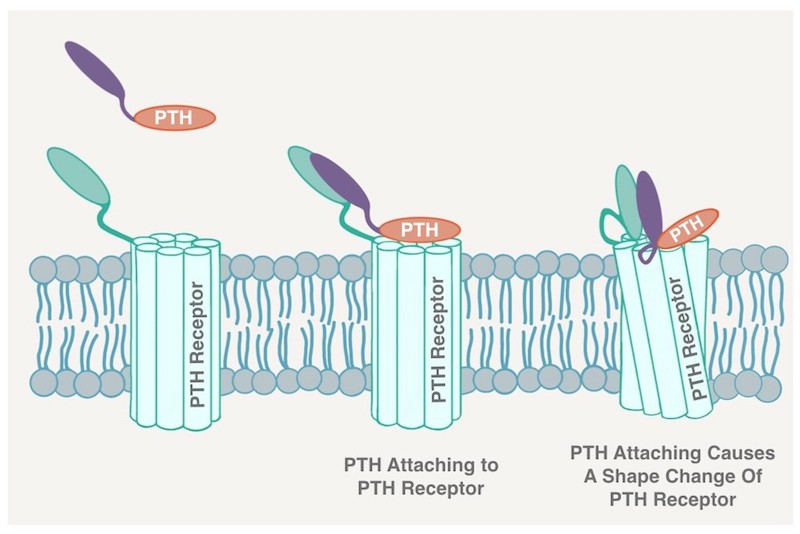
PTH is very interesting in and of itself. It is a 3D protein that has parts that attach to other proteins, called receptors, on the surface of other cells in a lock-and-key fashion. This is how PTH gives its instructions to other tissues like the bones and kidneys. PTH delivers a command, so it has been designed to disintegrate shortly after it has been released in the bloodstream. Half of the PTH proteins disintegrate within 5 minutes of going into the bloodstream. This ensures that if the parathyroids want to give a different command a few minutes later, then PTH is not hanging around in the blood to interfere with the new command. The rapid intraoperative PTH test done during surgery takes advantage of this short lifespan (also called a half-life). The parathyroid receptor is present in many different areas of the body, including the kidneys, bones, adrenal glands, cartilage, heart muscle, and nerve cells in various parts of the brain. When a person has hyperparathyroidism, some of the symptoms are due to high calcium in the blood, and others are directly from the PTH. In fact, some of the symptoms directly correlate with the level PTH in the blood.
Calcium and PTH on a Cellular Level
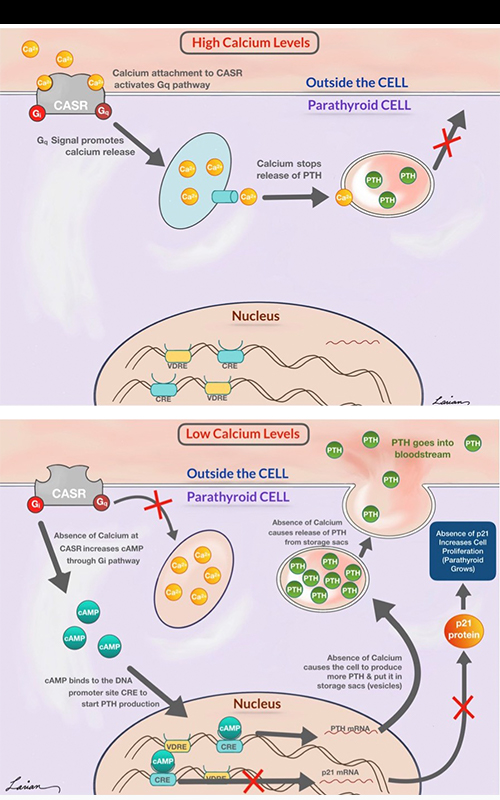
When calcium levels are high in the blood, they seep out of the blood vessels into the fluid surrounding cells. The calcium elements will then attach to the calcium sensing receptor (CASR) on the surface of parathyroid cells and start a series of reactions that ultimately result in stopping the release of PTH from the cells. In doing this, the PTH level in the bloodstream comes down, because whatever PTH was already in the blood will quickly disintegrate and disappear.
On the other hand, when calcium levels are low, and no calcium is attached to the CASR, another set of reactions occur that ultimately increase the PTH release outside of the cell and into the bloodstream. When low calcium levels happen for a short period of time, then the parathyroid cell will signal the sacs (vesicles) containing PTH to merge with the surface and release what is inside the sac (PTH). When the low calcium level goes on for an extended period of time, in addition to releasing the PTH containing sacs, the parathyroid glands send signals to the nucleus (brain of the cell) to start the process of manufacturing PTH and place it in the storage sacs. If the calcium level stays chronically low, then, through a different series of reactions (P21 protein), parathyroid cells are signaled to duplicate themselves (proliferate). Thus, the parathyroid gland may grow to keep up with the demands of the body.
Parathyroid Disease
If there is a disturbance in just a single cell on one of the parathyroid glands and the calcium levels are no longer being monitored properly, you will develop hyperparathyroidism. Watch the video below to learn about hyperparathyroid disease.
Parathyroid Gland FAQ
Q: What is considered a “normal” PTH level?
A: The average PTH level ranges from 10 and 65 pg/ml. If an individual’s PTH level rises above this range, he or she may be dealing with hyperparathyroidism.
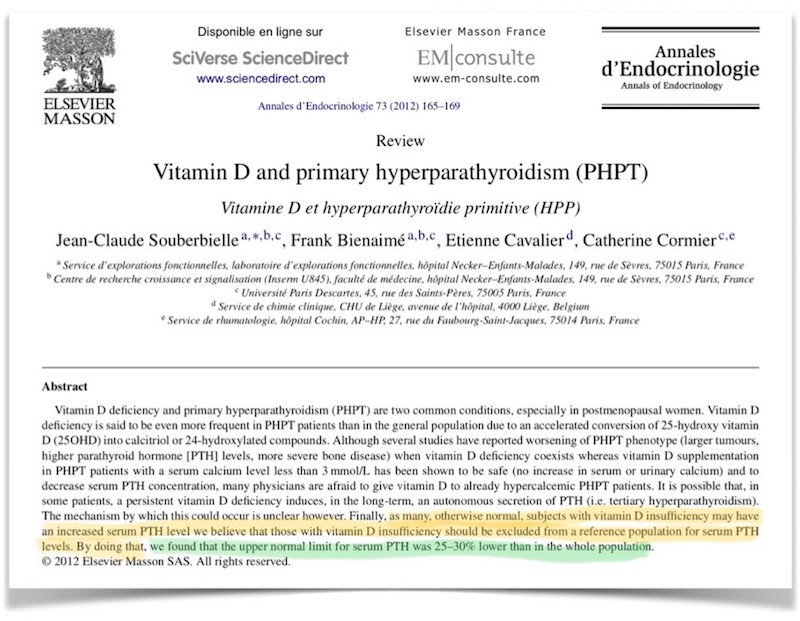
Q: Are the “normal” PTH level affected by vitamin D levels?
A: To start a large portion of healthy population (more than 60%)has vitamin D deficiency so when we say “normal” PTH level ranges between 15-65, it does include these patients. A higher proportion of patients with PHPT have vitamin D deficiency. Because vitamin D causes the parathyroid glands work less and causes lowering of PTH, if there is vitamin D deficiency then the range of PTH should be different as shown in the article below. It should be less by 25%, so the upper limit of normal for PTH in a person who has vitamin D levels higher than 30 ng/ml should be 48 pg/ml rather than 65 pg/m.
Q: Does chronic vitamin D deficiency cause hyperparathyroidism?
A: Yes, it can, and it is called secondary hyperparathyroidism. The thought is that since vitamin D suppresses the parathyroid glands, if vitamin D is deficient the parathyroid glands wont have vitamin D telling it to work less, and not grow; because of this parathyroid over react and cause secondary hyperparathyroidism.
Q: What causes a person’s calcium level to rise?
A: There are many reasons for calcium elevation. But the most common cause of high calcium in patients that are not hospitalized is parathyroid overactivity. PTH effect in the bones, gut, and kidneys causes elevated calcium level.
Q: Can an elevated calcium level contribute to parathyroid cancer?
A: No, persistent elevation in calcium does not cause parathyroid cancer. Parathyroid cancer develops as a consequence of mutations in the genes inside a parathyroid gland. Parathyroid cancer patients generally have a rapidly elevating calcium level, as well as very high PTH levels. Yet parathyroid cancer is rare, and it affects less than 1% of primary hyperparathyroidism patients.
Q: Are foods available to help promote good parathyroid health?
A: Foods that contain calcium and vitamin D often promote good parathyroid health. Calcium-rich foods include milk, cheese, yogurt, spinach, and broccoli. Also, vitamin D-rich foods include fish, mushrooms, and beef liver. All of the aforementioned foods can be integrated into a person’s diet.
Parathyroid Gland Surgery
Parathyroid gland surgery may be required if the parathyroid glands stop functioning properly. Oftentimes, it is difficult to identify parathyroid disease symptoms. Thanks to blood calcium tests, an individual can find out if he or she is dealing with hyperparathyroidism.
If a blood calcium test reveals elevated blood calcium levels, a doctor may perform additional tests to verify his or her results. Then, if a doctor believes an individual is a good candidate for parathyroid gland surgery, he or she crafts a custom hyperparathyroidism treatment plan.
Choose the Right Surgeon to Perform a Parathyroid Gland Procedure
Dr. Babak Larian of the CENTER for Advanced Parathyroid Surgery is an expert head and neck surgeon. He understands the intricacies of minimally invasive head and neck procedures and is happy to share his surgery insights with patients. That way, patients can receive comprehensive support and guidance throughout the parathyroid surgery cycle.
Dr. Larian is available to meet with an individual to assess his or her parathyroid gland function and offer personalized treatment recommendations. To schedule a consultation with Dr. Larian, please call us today at 310-461-0300.









