"*" indicates required fields
Understanding Hyperparathyroidism and Vitamin D Deficiency
You need to understand hyperparathyroidism, vitamin D deficiency, and elevated calcium levels — how they relate to each other and what that means for you.
Why? Because you have been feeling off for a long while — low energy, foggy thinking, trouble sleeping. Your doctor tells you that your vitamin D levels are low, and you might have hyperparathyroidism. That doesn’t seem so bad; maybe you can spend more time in the sunshine or take supplements. But the doctor is recommending surgery.
Before you make any decisions, it helps to understand what’s going on inside your body.
That starts with a clear explanation of how the parathyroid glands work in a healthy system—and what happens when vitamin D levels fall out of balance. We’ll see how vitamin D levels drop due to primary hyperparathyroidism (PHT) and how a vitamin D deficiency can trigger secondary hyperparathyroidism (SHPT).
Let’s get started.
How the Parathyroid Glands, Calcium, and Vitamin D Work Together
Before tackling the connection between hyperparathyroidism and vitamin D deficiency, let’s first look at how the parathyroid glands work in a healthy body.
You have four parathyroid glands, each similar in size to a grain of rice, that can be found in your neck behind the thyroid. Their job is simple but essential: they regulate the calcium level in your bloodstream.
Calcium does more than help build strong teeth and bones. It also helps regulate your heartbeat, control muscle contractions, support nerve communication, aid blood clotting, and assist in hormone release.
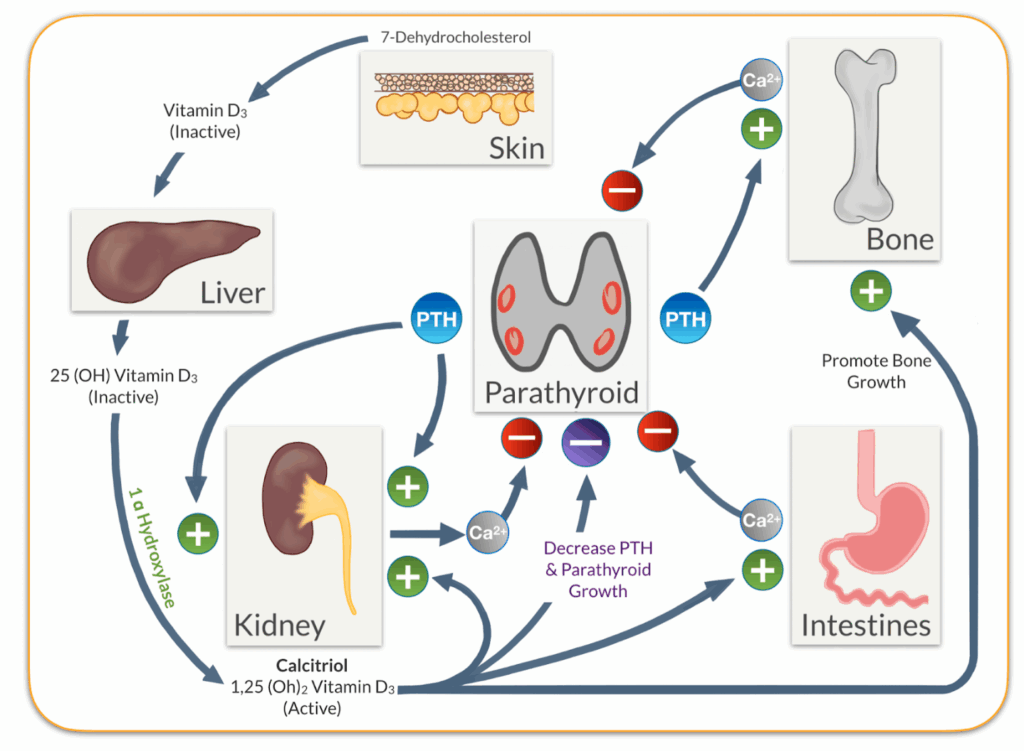
But calcium levels must stay within a very narrow range. When the amount of calcium in your blood gets too high or too low, your body cannot function properly. That’s where the parathyroid gland steps in. When calcium levels drop, the parathyroid gland produces more parathyroid hormone (PTH), which acts on three main systems to bring the calcium levels back up:
- Bones: PTH triggers the release of small amounts of calcium from your bones into your bloodstream.
- Kidneys: It causes your kidneys to conserve calcium rather than flushing it out through urine.
- Intestines: Indirectly, PTH tells your kidneys to activate vitamin D. Active vitamin D helps your intestines absorb more calcium from the food you eat.
Once your calcium levels rise back to normal, the parathyroid glands slow the production of PTH. It’s a tight, well-calibrated feedback loop that your body constantly adjusts to, minute by minute, maintaining a calcium balance.
Hyperparathyroidism results when this system is disrupted:
- In primary hyperparathyroidism (PHPT), a benign tumor develops, causing one of the parathyroid glands to produce too much PTH, increasing calcium levels even when they are already high. Vitamin D levels often drop as the body tries to limit additional calcium absorption.
- In secondary hyperparathyroidism (SHPT), a vitamin D deficiency impairs your body’s ability to absorb calcium from the food you eat. This causes the parathyroid glands to produce more and more PTH as they attempt to correct the imbalance.
As you can see, the relationship between hyperparathyroidism, vitamin D levels, and calcium is both intricate and essential to a healthy body.
Many people don’t realize they have a problem until hyperparathyroid symptoms take a toll or routine blood work raises a red flag. Often, the first clue is a calcium imbalance or low levels of vitamin D. Understanding how vitamin D works and how, if deficient, it can lead to a diagnosis of hyperparathyroidism can help you ask the right questions to stay well-informed.
Diagnosing Hyperparathyroidism: The Role of Vitamin D Levels
Before exploring the mechanism between vitamin D deficiency and hyperparathyroidism, let’s take a closer look at how vitamin D functions in a healthy body.
Understanding Vitamin D
Vitamin D’s main function in the body is to help the intestines absorb calcium, but it does a lot more.
Since vitamin D, calcium levels, and parathyroid gland function are intimately involved. To understand this relationship better, we have to first discuss how the body creates and activates vitamin D. There are two ways the body makes the chemical that ultimately becomes vitamin D:
- By using sunlight (UVB) to transform cholesterol to inactive vitamin D (cholecalciferol) or
- By ingesting vitamin D2 or vitamin D3 in our diet.
Both of these processes are usually working simultaneously for each of us.
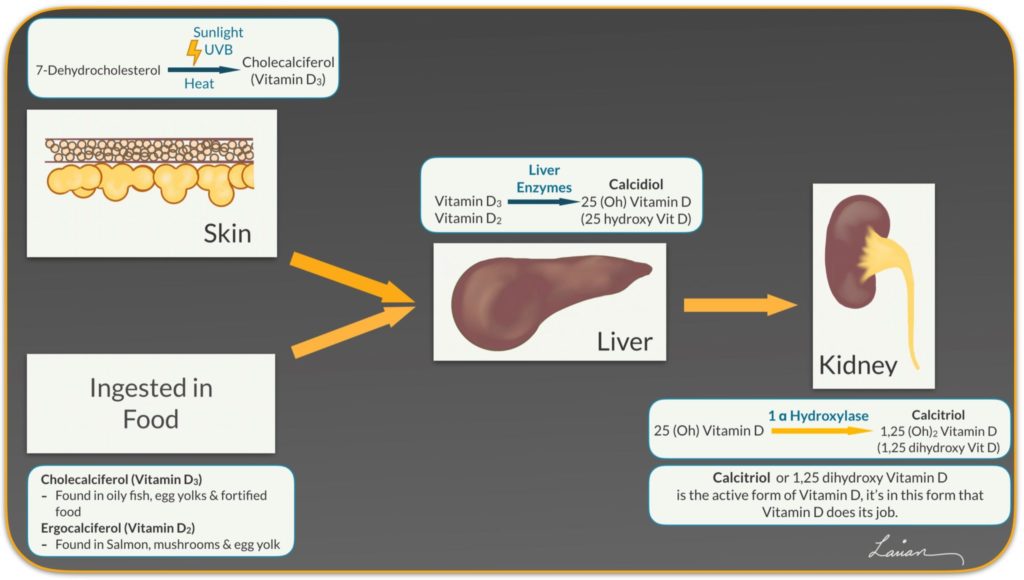
These forms of vitamin D then pass through the liver, where they are transformed into calcidiol (also known as 25-hydroxyvitamin D). From there, this inactive form of vitamin D travels through the bloodstream to the kidneys.
In the kidney, parathyroid hormone (PTH) stimulates the activation of vitamin D3 into its useable form, called calcitriol, also known as 1,25-dihydroxyvitamin D3.
Activated vitamin D3 enters the bloodstream and travels throughout the body. It affects the calcium balance in several key ways:
- It has the most impact on calcium absorption in the small intestines.
- It also causes the kidneys to absorb more calcium from urine.
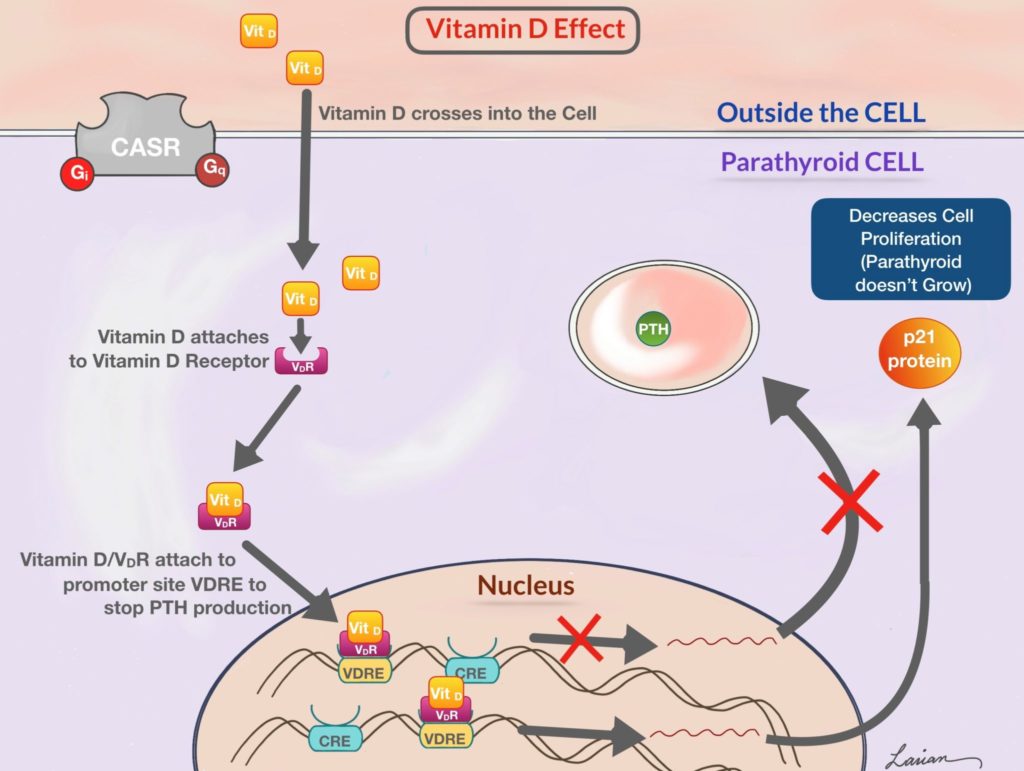
- It causes the parathyroid glands to make less PTH.
- It causes the bones to release calcium and phosphorus in small amounts.
- It helps mature the cells that make and reshape bone, making it stronger.
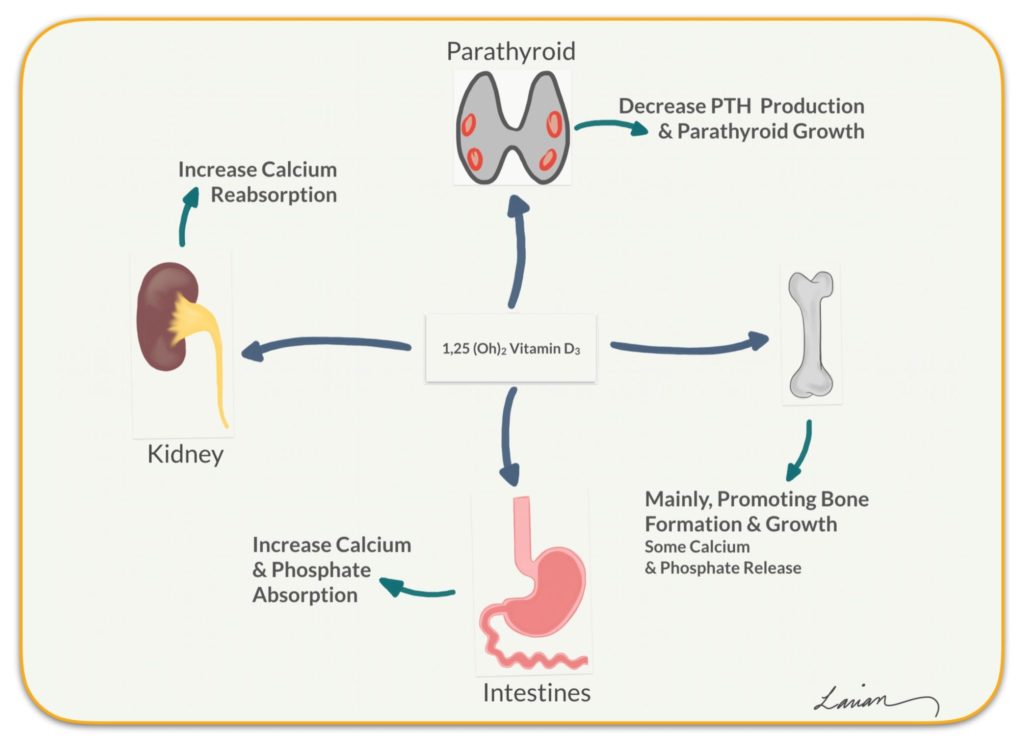
On a cellular level, vitamin D enters parathyroid cells and stops the production of PTH. It also promotes the production of a protein called p21. The p21 protein stops the parathyroid gland from duplicating and essentially helps keep the gland from growing.
Other Potential Benefits of Vitamin D
Vitamin D has been shown to be involved in many other bodily processes. The following is a list of potential benefits of vitamin D; I say possible because not all of these have been clearly proven.
- Boosting immunity
- Reducing cardiovascular risk
- Supporting a healthy pregnancy
- Reducing the risk of Alzheimer’s disease
- Protecting against diabetes
- Reducing inflammation
- Combating depression
- Reducing the risk of cancer
How Vitamin D Deficiency Affects Calcium and PTH
A vitamin D deficiency is a condition in which an individual doesn’t have sufficient vitamin D in the body. When vitamin D levels are low, calcium absorption in the intestines decreases, which causes the blood calcium level to lower. Consequently, the parathyroid glands become more active and produce more PTH. This causes calcium to come out of the bones, weakening them over time. A vitamin D deficiency may cause a wide range of health problems if left unaddressed for an extended period.
There are many reasons why someone may become vitamin D-deficient, including:
- Lack of vitamin D-rich foods in the diet
- Malabsorption issues that make it difficult for the body to absorb vitamin D from food
- Limited sun exposure
- Liver or kidneys that struggle to convert vitamin D into its active form
- Medications that disrupt the body’s ability to convert or absorb vitamin D
Some individuals are more prone to vitamin D deficiencies than others, including:
- Older Adults: As we age, the skin becomes less effective in absorbing vitamin D from sunlight.
- People with Dark Skin: Darker skin is an adaptation to protect against the harmful effects of too much sun exposure, which also means there is less UVB light available to make vitamin D. Typically, people with darker skin need more sun exposure than those with lighter skin to make sufficient vitamin D. In the modern era of indoor living and work, we are all exposed to less sunlight.
- People with Obesity: Vitamin D is fat-soluble, meaning it can be stored in fat tissue. Excess body fat can bind vitamin D, preventing it from reaching the blood.
The American Academy of Pediatrics recommends that children and infants receive at least 400 IU of vitamin D daily from diet and supplements. Meanwhile, research shows that adults who consume 700 to 800 IU of vitamin D daily are less prone to bone fractures.
Testing for Vitamin D Deficiency and Hyperparathyroidism
People with hyperparathyroidism often find that their vitamin D level is affected as well. That’s why checking vitamin D levels is part of the diagnostic process. The primary way to diagnose vitamin D deficiency is with a 25-hydroxyvitamin D blood test. During this test, a doctor measures the amount of vitamin D present in a person’s body.
If your vitamin D level is less than 20 ng/mL, you will be diagnosed as vitamin D-deficient based on the American Institute of Medicine guidelines. The Endocrine Society considers levels lower than 30 ng/mL to be a deficiency of vitamin D.
If your test shows you are vitamin D-deficient, there is no need to panic. A doctor will work with you to identify the root cause of the deficiency and develop a personalized treatment plan.
How to Treat a Vitamin D Deficiency
Dietary changes and the use of supplements often help people overcome vitamin D deficiencies.
Many foods naturally contain high levels of vitamin D, including:
- Beef liver
- Fatty fish (salmon, tuna, sardines, trout, and mackerel)
- Fish Oil
- Cheese
- Egg yolks
- Mushrooms (Shiitake)
Vitamin D helps the body absorb calcium more readily. This is why milk is commonly fortified with vitamin D. Otherwise, your body wouldn’t be able to absorb the calcium in the milk. Other foods fortified to contain high levels of vitamin D include:
- Cereal
- Orange juice
- Yogurt and other dairy products
Vitamin D supplements are available in both pill and liquid forms. Regular monitored use can help address a vitamin D deficiency.
Those who are vitamin D deficient should meet with a doctor before making dietary changes or using supplements. It’s crucial to work with a medical professional to determine a safe and effective way to treat the deficiency.
Vitamin D and vitamin K2 are complementary vitamins. While vitamin D is necessary for absorbing calcium from food in the intestines, vitamin K2 does two functions that help direct the calcium where it’s needed:
- By activating osteocalcin, a protein that promotes the accumulation of calcium in bones and teeth, and
- By decreasing the accumulation of calcium in soft tissues, such as the kidneys and blood vessels
Vitamin K2 is found in beef liver, egg yolk, soft cheese, and fermented foods.
Is It Possible to Consume Too Much Vitamin D?
We know that vitamin D deficiency can lead to hyperthyroidism, but can you have too much vitamin D?
Yes, it is possible to consume too much vitamin D. Because vitamin D is fat-soluble, we can store extra vitamin D in our fat tissue, which can build up over time. Vitamin D is one of four vitamins that can accumulate in the body to toxic levels. Water-soluble vitamins are disposed of in the urine (part of the reason urine changes color with excessive vitamin use). Unfortunately, that doesn’t happen with vitamin D. Excess consumption of vitamin D is problematic; the levels can become toxic, and it may cause any of the following symptoms:
- Nausea
- Vomiting
- Constipation
- Lack of appetite
- Weakness
- Weight loss
High levels of vitamin D may also increase calcium levels in the blood, which can cause confusion, disorientation, and heart rhythm issues.
How Vitamin D Deficiency Contributes to Hyperparathyroidism Symptoms
When a person has a vitamin D deficiency for a long time, the parathyroid glands respond by increasing the production of PTH. This prompts the bones to release more calcium into the bloodstream. This may cause only a mild elevation in calcium or none at all. However, it can still cause bone loss and symptoms of hyperparathyroidism to occur. This is secondary hyperparathyroidism (SHPT), secondary due to vitamin D deficiency.
Generally, SHPT can be easily corrected by restoring vitamin D levels with supplements, which will lead to PTH levels coming back to normal.
What Is the Link Between Primary Hyperparathyroidism and Vitamin D Deficiency?
Vitamin D deficiency is common in today’s society, but it is significantly more common in people who have primary hyperparathyroidism.
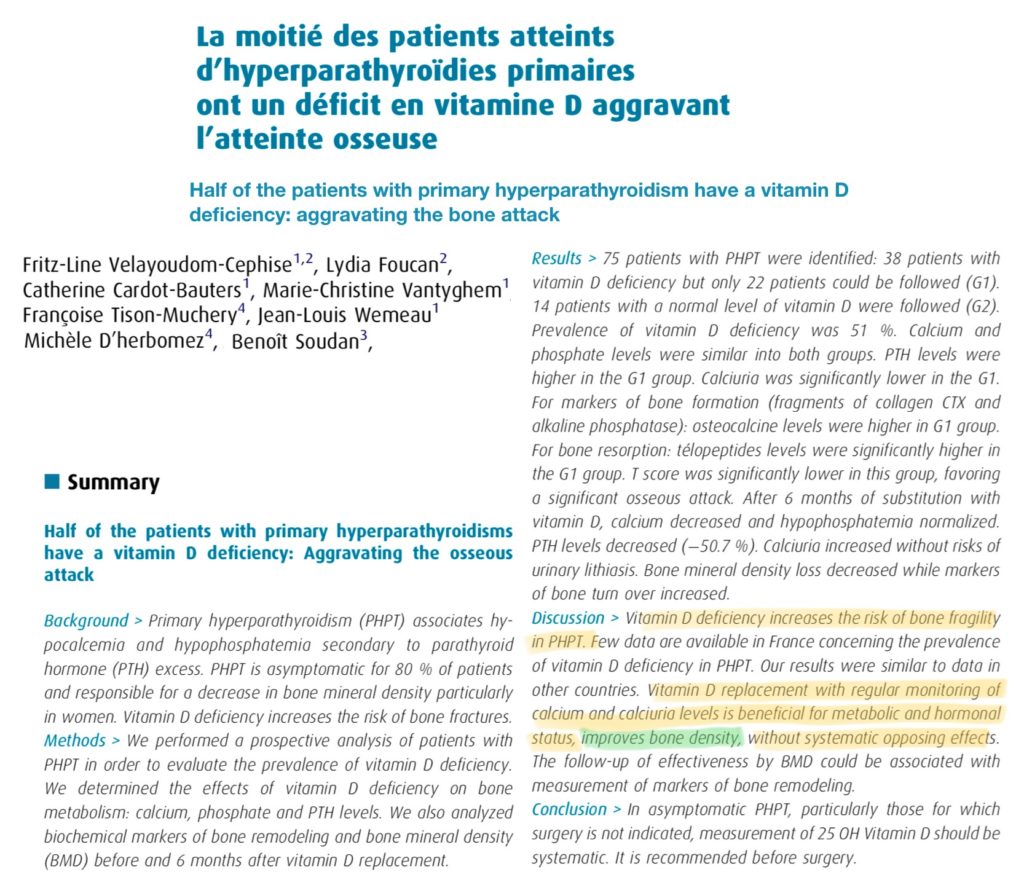
Someone with primary hyperparathyroidism and vitamin D deficiency is likely to experience more severe symptoms, including a higher rate of bone loss or osteoporosis.
Patients with hyperparathyroidism and low vitamin D will likely experience the following effects that those with hyperparathyroidism and normal vitamin D will not:
- More frequent bone fractures
- Larger parathyroid tumors (adenomas)
- A higher PTH level
- Increased markers of bone turnover (an early sign of bone loss)
The reason vitamin D deficiency in hyperparathyroidism is so common is not clear. Some theorize it’s because the higher PTH level increases the conversion of 25-hydroxyvitamin D to its active form, 1,25-dihydroxyvitamin D.
It is likely that other processes are occurring in the body that decrease vitamin D levels to protect the body against higher calcium levels. The exact mechanism remains unclear. The bottom line? Vitamin D deficiency can cause many problems and needs to be treated appropriately.
Studies have also revealed that large adenomas, high PTH levels, and more severe bone disease are more common in patients with hyperparathyroidism and vitamin D deficiency compared to those with isolated vitamin D deficiency.
When vitamin D levels are low:
- The parathyroid gland is not suppressed and can grow larger. PTH production is not inhibited, so the level is higher (leading to more symptoms), and
- Bones are less protected, leading to more bone loss.
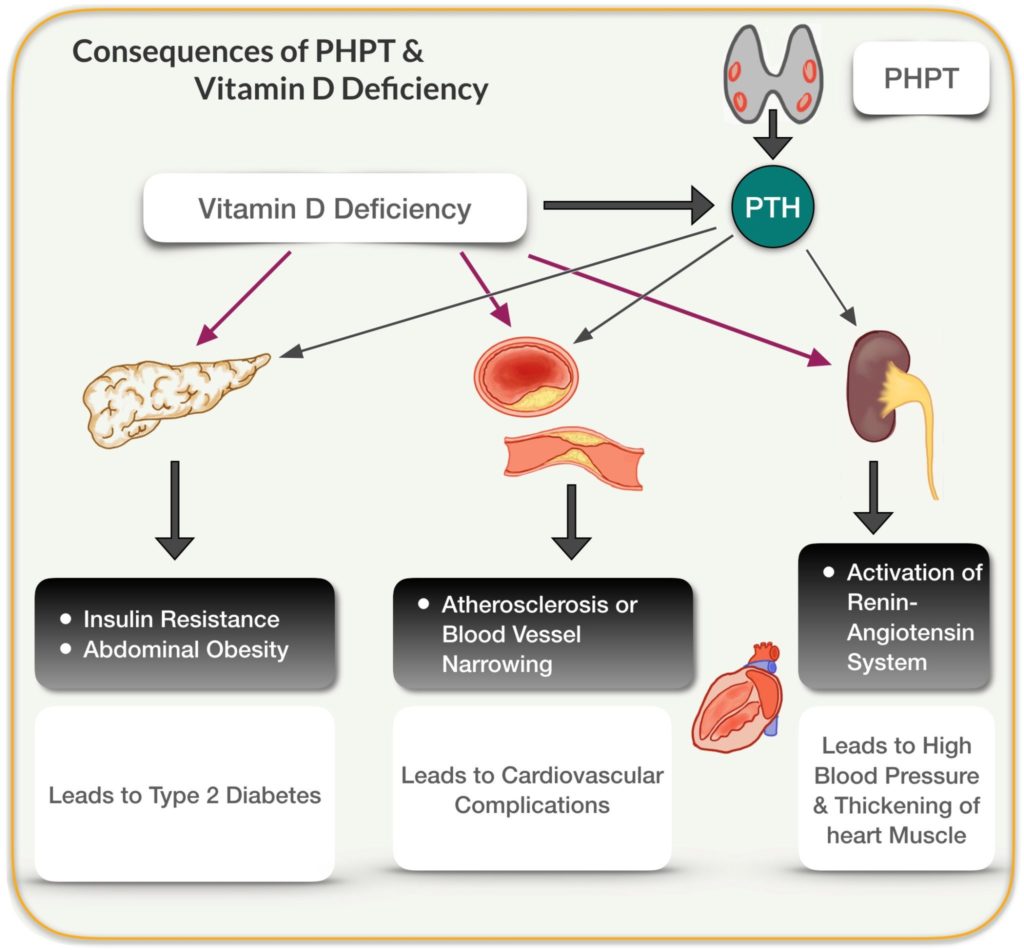
The combination of primary hyperparathyroidism and vitamin D deficiency has effects on other systems too, including the pancreas and insulin, blood vessels, and kidneys, leading to many other complications.
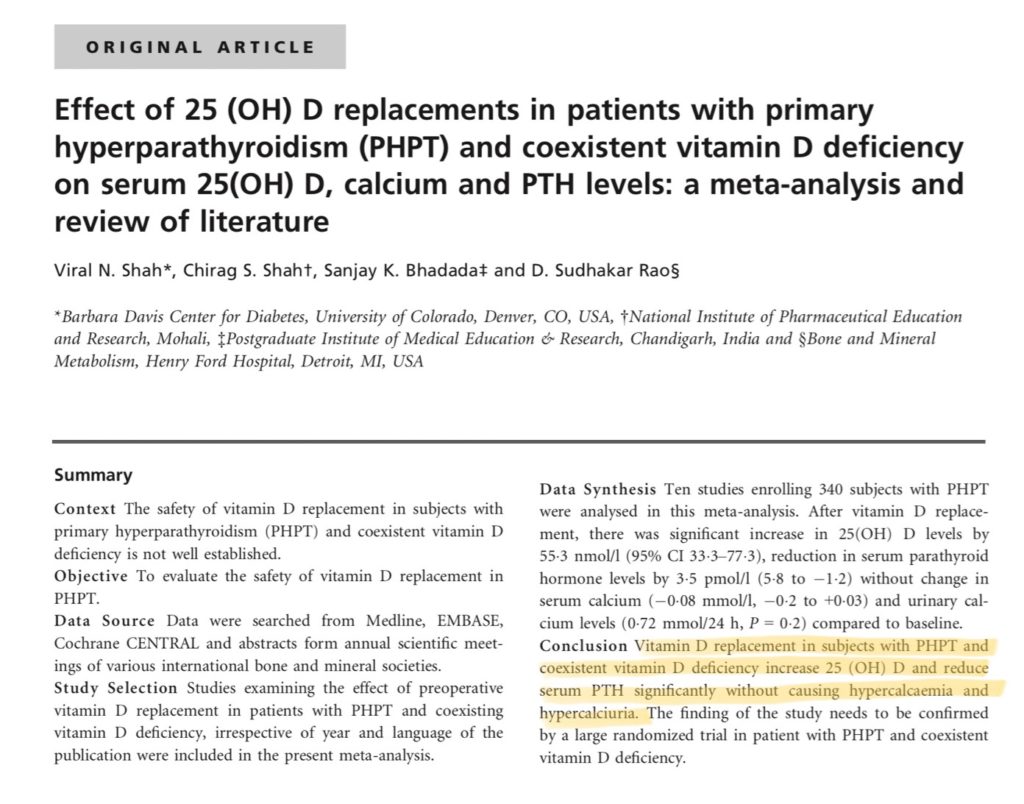
Although some still worry that vitamin D replacement is dangerous and can cause problems, the research is clear. When vitamin D is replaced in a controlled manner with the help of a doctor and lab testing, it can be very safe. Additionally, replacing vitamin D does not cause elevation in blood or urine calcium, and it helps reduce elevated PTH levels.
Vitamin D and Hyperparathyroidism: Effective Treatment Options
In a great number of cases, blood tests show that a person’s inactive vitamin D level (25-hydroxyvitamin D or 25 OH Vit D) is low, but their active vitamin D level (1,25-dihydroxyvitamin D or 1,25 OH Vit D) is normal or even high. This happens because elevated PTH increases the conversion of the inactive vitamin D into its active form.
Between active and inactive vitamin D levels, it’s easy to miss what’s really going on. Your test may show low vitamin D levels. But if you have hyperparathyroidism and vitamin D deficiency, your body may already be converting inactive vitamin D into high levels of the active form (1,25-dihydroxyvitamin D), even if the blood test shows that your total vitamin D is low.
Some patients with hyperparathyroidism and vitamin D deficiency can experience improved bone health and lower PTH levels by taking carefully monitored vitamin D supplementation under a physician’s supervision.
Some patients with hyperparathyroidism and vitamin D deficiency can increase their vitamin D levels by taking daily or weekly supplements. However, some will find that taking vitamin D supplements makes them feel worse. This may happen because the high PTH rapidly converts the supplements into high concentrations of its active form, causing symptoms of vitamin D toxicity.
When taking vitamin D makes you feel worse, stop taking it immediately and consult your doctor.
In either scenario, parathyroidectomy will not only correct the calcium/PTH imbalance (hyperparathyroidism) but also the vitamin D deficiency.
All in all, it is important to seek treatment for hyperparathyroidism, no matter your vitamin D level. The high level of calcium in the blood, caused by the overactive parathyroid glands, can have detrimental long-term effects on the kidneys, bones, muscles, and other organs. Many patients will live with hyperparathyroidism for quite some time without knowing they have the condition. When symptoms do present, most patients benefit greatly from the removal of the abnormal parathyroid gland(s).
In a procedure known as a minimally invasive parathyroidectomy, Babak Larian, MD, FACS, uses endoscopic technology and a small incision to remove the affected parathyroid gland. Through the use of intra-operative PTH testing, he can be certain the procedure is successful before closing up the incision. Most patients who were experiencing symptoms of hyperparathyroidism and vitamin D deficiency before surgery experience great relief almost immediately following.
Schedule a Parathyroid Disease Treatment Consultation with Dr. Larian Today
If you have any questions about the connection between hyperparathyroidism and vitamin D, or are living with the symptoms of hyperparathyroidism, Dr. Larian can help. Contact us today at the Center for Advanced Parathyroid Surgery or call 310-461-0300 to schedule a consultation.
Hyperparathyroidism and Vitamin D FAQs
Vitamin D replacement in the setting of PHPT has been shown to have positive impact when monitored by your physician.
Q: Is it safe to take vitamin D supplements if I have primary hyperparathyroidism?
A: Yes, as long as the vitamin D levels are being monitored by your physician. If you feel worse or have new, uncomfortable symptoms, stop immediately and have your blood levels checked.
Q: Does taking vitamin D supplements protect my bones if I have primary hyperparathyroidism (PHPT)?
A: Yes. In patients with primary hyperparathyroidism and vitamin D deficiency, carefully monitored supplementation can help reduce bone loss and improve overall bone health.
Q: What do I do if taking vitamin D supplements makes me feel worse?
A: Stop taking the supplement immediately and contact your doctor. It is important to get blood tests to check calcium, PTH, 25-OH vitamin D, and 1,25-OH vitamin D to see if you are experiencing vitamin D toxicity and to understand its impact on your parathyroid function.
Q: Is it safe to take calcium replacement when you have PHPT?
A: It’s unclear. Research is limited. Most experts advise against taking calcium supplements with PHTH unless directed by your physician.









