Hyperparathyroidism happens when one or more parathyroid glands over produce their hormone (PTH) and cause an imbalance in the blood calcium level. To understand how this happens you have to know how the parathyroid glands normally function.
The main job of the parathyroid glands is to monitor the blood to make sure the correct amount of calcium is in the blood stream, or in other words keep the level calcium in the blood a constant number or close to it. This is done so that the rest of the body that uses calcium always knows how much is available in the blood. The parathyroids work tirelessly day & night to do this. They are very successful at their job, that is why the calcium levels only briefly will go much higher or lower then the intended level, and are quickly brought back to the body’s expected level.
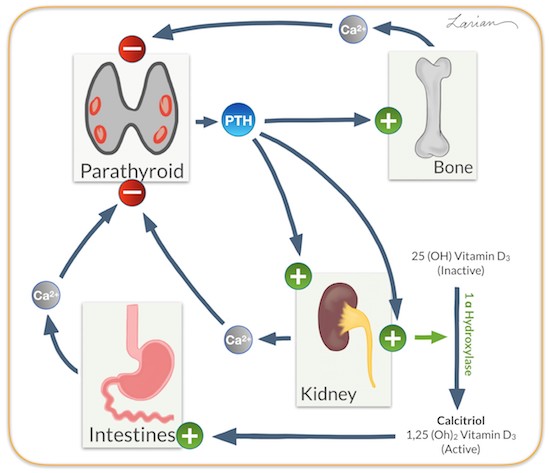
They do this by producing parathyroid hormone or PTH when blood calcium level is low. PTH goes to the bones (the main storage area of calcium), and tell the bone to release calcium into blood. PTH goes to the kidneys (main calcium filtration system) and tells the kidney to get the calcium out of urine and put it back into the blood; in the kidney they also activate vitamin D. Active vitamin D goes to the intestines and helps the absorb more calcium from the food. When the calcium level comes up, the gland stops producing PTH. This is a feedback loop, that essentially controls itself to keep your blood calcium at a level that your particular body wants. Your body wants your calcium to be a set number all your life and can tolerate only short periods of time when its higher or lower.
What is Primary Hyperparathyroidism?
The parathyroid gland has a calcium sensor on the surface of the parathyroid cells that is genetically set for a certain calcium level, like a thermostat temperature setting (9.0 in Figure 1).
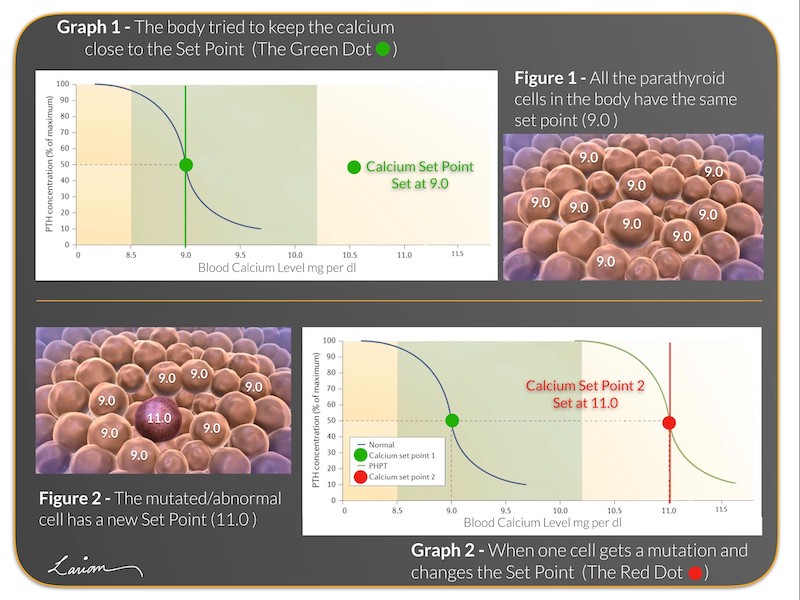
In primary hyperparathyroidism tumor develops within a parathyroid gland when there is a disturbance on the calcium sensor of a single parathyroid cell; this changes the setting for the calcium to a higher number (11.0 in Figure 2) for that particular cell, while the remaining normal cells stay at the proper level.
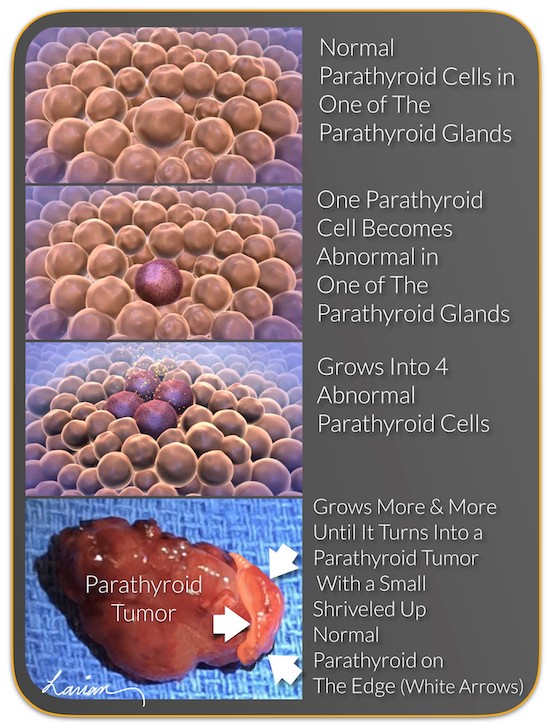 However, as the calcium in the blood increases, the normal parathyroid cells “turn off,” while the abnormal or bad parathyroid cell continues to produce PTH.
However, as the calcium in the blood increases, the normal parathyroid cells “turn off,” while the abnormal or bad parathyroid cell continues to produce PTH.
The abnormal parathyroid cell begins to multiply and get bigger and the normal cells that are currently not active start to get smaller and shut down. Over time, the calcium level will increase until it reaches the set point of the parathyroid tumor cells. Because primary hyperparathyroidism is caused by the abnormality of the sensor, the elevated calcium level will continue to stay at the new level as long as the parathyroid tumor is in the body. Essentially the parathyroid tumor hijacks the calcium control system.
This can lead to a variety of debilitating symptoms, including:
- Weakening of the bones, causing osteoporosis and bone fractures;
- Kidney stones, which can harm the overall function of the kidney;
- Sluggish nervous system, leading to fatigue, memory loss, poor concentration, anxiety, and depression;
- Stiffening of the blood vessels and high blood pressure;
- Rhythm abnormalities in the heart and heart palpitations;
- Intestinal issues such as acid reflux and constipation.
If left untreated for too long, hyperparathyroidism can significantly reduce your life expectancy and increase your risk of certain cancers, such as colon cancer, kidney cancer, breast cancer, and prostate cancer. Unfortunately there is no medication to cure hyperparathyroidism, but rather medications are available that can be taken in combination for a lifetime to control it; the only cure is surgery.</p
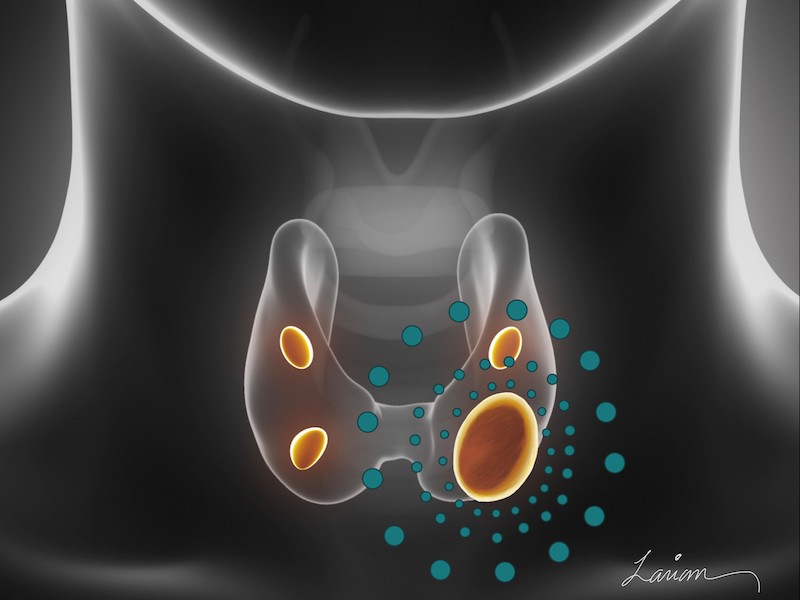
The majority of the time, a parathyroid tumor is located in 1 of the 4 parathyroid glands. It is usually a benign tumor, called a parathyroid adenoma, which grows to an abnormal size. As it grows it releases greater amounts of PTH, thus causing Primary Hyperparathyroidism (PHPT).
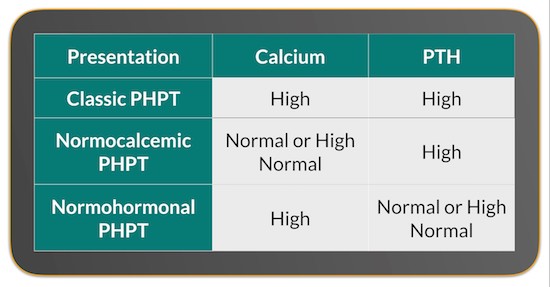
Primary hyperparathyroidism or PHPT presents in many different ways. The most well known presentation is the classic or hypercalcemic primary hyperparathyroidism. This is when both the calcium and PTH are elevated. But equally important are the unusual presentations which include normocalcemic PHPT, with normal calcium and elevated PTH; normohormonal PHPT that has high calcium with normal PTH levels. The nonclassic laboratory version of PHPT (normocalcemic or normohormonal) can be harder to diagnose & require some degree of expertise.

Who gets Hyperparathyroid Disease?
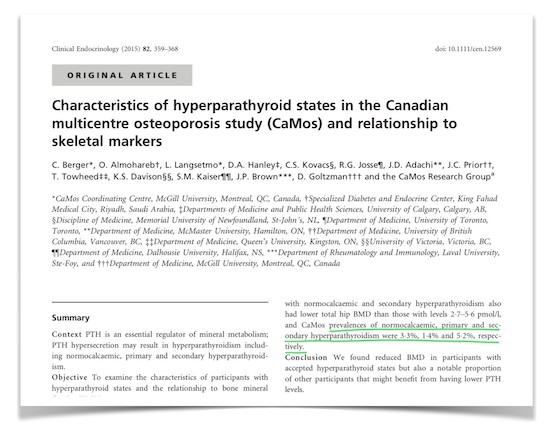
100,000 new cases of PHPT are diagnosed every year. In the United States it has been estimated 1 in every 800 people has PHPT, with the disease being more common in women, affecting 1 in every 250 women over the age of 60. However, in a Canadian osteoporosis study it was found in more then 4.5% of the adults over the age 35. Unfortunately, the majority of those who have hyperparathyroidism are not diagnosed or are misdiagnosed, as PHPT is a complex or confusing disease for inexperienced physicians.
“I struggled unsuccessfully for months to find a local surgeon who could diagnose my hyperparathyroidism, and was fortunate enough to learn about Dr. Larian while doing my own research. Few doctors are knowledgeable about parathyroid disease, even fewer can perform the surgery successfully using minimally invasive procedures.” –Jennifer, Washington DC
Parathyroid Adenoma Vs. Hyperplasia
The most common reason for hyperparathyroidism is a benign (noncancerous) tumor called parathyroid adenoma. 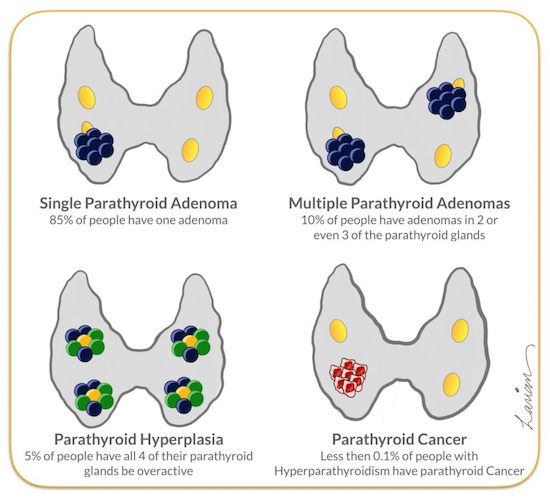 A parathyroid adenoma (or bad parathyroid gland) is a growth inside a parathyroid gland that causes the gland to produce excessive amounts of parathyroid hormone (PTH). Because the tumor forces the gland to make more and more PTH, the calcium levels in the blood increase, which is known as hypercalcemia. While a single adenoma is most common, it is possible to have parathyroid adenomas on several glands.
A parathyroid adenoma (or bad parathyroid gland) is a growth inside a parathyroid gland that causes the gland to produce excessive amounts of parathyroid hormone (PTH). Because the tumor forces the gland to make more and more PTH, the calcium levels in the blood increase, which is known as hypercalcemia. While a single adenoma is most common, it is possible to have parathyroid adenomas on several glands.
While the vast majority of patients only have a single parathyroid adenoma, it is very important to still conduct a 4 Gland Assessment to guarantee the patient is cured. Whether you have 1 parathyroid adenoma or 3 parathyroid adenomas, the signs and symptoms will be the same. Symptoms are not necessarily more extreme when a patient has multiple adenomas.
Over time the parathyroid tumor will continue to grow and your parathyroid disease will get worse until the tumor is removed. At the same time, your remaining normal parathyroid glands will stop working and can shrink in size over time. A parathyroid tumor will never go away on it’s own; it must be surgically removed. When performed by an expert parathyroid surgeon, like Dr. Larian, a minimally invasive parathryoidectomy is quick and successful cure for parathyroid tumors.
Interesting Parathyroid Adenoma Facts
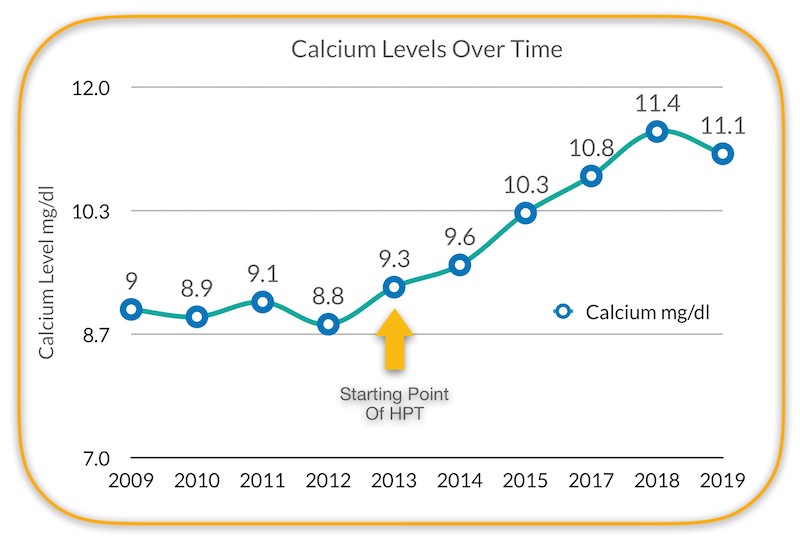
- Primary hyperparathyroidism develops over a period of years.
- Calcium elevation usually plateaus with parathyroid adenomas, even though PTH levels continue to elevate.
- Calcium levels do not correlate to the size of the parathyroid adenoma.
- The size and weight of abnormal parathyroid gland(s) is directly proportional to PTH levels and inversely proportional to Vitamin D levels.
- Degree and severity of hyperparathyroid symptoms does not always correlate to calcium levels.
- Bone mass density loss occurs with all forms of hyperparathyroidism, even in Normocalcemic Hyperparathyroidism.
- Bone mass density usually presents after 8 or more years of the disease process.
“After years of vague symptoms and months of severe symptoms, just days after surgery I feel better than I have in such a long time.” -Jennifer
What Are the Causes of Hyperparathyroidism?
Primary hyperparathyroidism, is called primary because the source of the problem is primarily in the parathyroid gland itself. The causes include:
- A noncancerous growth on one or two of the parathyroid glands
- Abnormal growth (hyperplasia) of all parathyroid cells in all parathyroid glands
- Very rarely a cancerous tumor in one the parathyroid gland
Secondary hyperparathyroidism is caused by other medical problems causing the parathyroid glands to secondarily overwork. Usually when the medical problem is corrected the hyperparathyroidism gets fixed. Common reasons why people experience secondary hyperparathyroidism include:
- Calcium deficiency
- Vitamin D deficiency
- Chronic kidney failure
Furthermore, people may be more prone than others to primary or secondary hyperparathyroidism if they fall into any of the following categories:
- Have received radiation treatment for cancer that exposed the neck to radiation, or for Grave’s Disease. Or radiation exposure, such as living in the area close to Chernobyl or Fukushima
- People who have used the medication lithium
- Have multiple endocrine neoplasia, type 1 or other rare inherited disorder
Hyperparathyroidism Symptoms
| System | Hyperparathyroidism Symptoms |
|---|---|
| Neuro-Psychiatric |
|
| Musculoskeletal |
|
| Gastrointestinal |
|
| Renal |
|
| Cardiac |
|
| Aesthetic |
|
Do You Need Parathyroid Surgery?

If you are suffering from hyperparathyroidism, the only cure is to find and remove the offending gland. Dr. Larian is a world-renowned parathyroid surgeon who helps patients feel like themselves again. Don’t wait any longer to be properly diagnosed with hyperparathyroid disease; help is available.
Hyperparathyroidism FAQ
- Are the symptoms of hyperparathyroidism different if you have an adenoma vs. multiple adenomas vs. parathyroid hyperplasia? No, the symptoms are the same for any of the different ways hyperparathyroidism occurs
- Can you tell from the size of the parathyroid adenoma how long you have had hyperparathyroidism? No
- Can you tell from the calcium level how long you have had hyperparathyroidism? No
- How can you find out how long you have had this disease? The only way to be certain is to look back in time at your previous calcium blood tests from a long time ago and see when the calcium started to come upwards.
- Are all the symptoms caused by the higher calcium levels? Not exactly, most symptoms come from calcium being higher in the blood, but a lot of the symptoms come from high PTH levels directly. PTH can act directly on nerves and in the brain, among other areas.
- Can you have symptoms when your calcium level is not very high? Absolutely
- Can you have symptoms if you have normocalcemic HPT, with your calcium levels in the normal range? Yes
- Can you get kidney stones or osteoporosis when your calcium level is only minimally elevated or if you have normocalcemic HPT?
Absolutely - When you have HPT and calcium levels are slightly raised, does it ever happen that your calcium can go back to normal? Yes, calcium is constantly changing, as our body’s needs & consumption change so does the calcium level. Even in the elevated calcium state, if that number is in the vicinity of normal , there can be occasions when the number goes down into the normal range. But it is not only the calcium level that tells you the story; it’s the relationship between calcium & PTH that is more telling. If the calcium goes back down in the high normal range but the PTH doesn’t come down into the low normal range ( Blue Dot), then the relationship is still not normal.
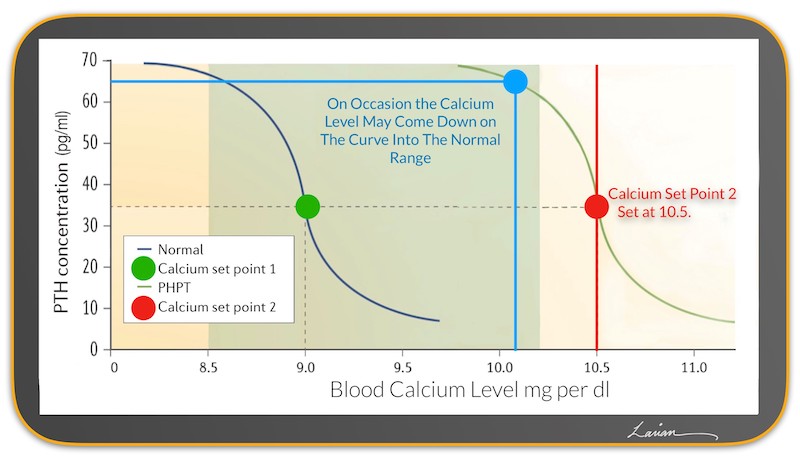
- If your calcium as in the example above goes back down to normal, will it remain in the normal range forever? Unfortunately not. It will at some point go back up again following the curve of PHPT towards the red dots.
- Can you have hyperparathyroidism and not have any symptoms? Yes, if the person has absolutely no symptoms, and feels mentally sharp, without fatigue, and has no body pains, then I would do a bone density scan & scans to look for kidney stones. If all the scans are normal then I would suggest they monitor their labs yearly and check bone density studies every 2 years; as long as these don’t change significantly then monitoring would be a good idea. The person may still choose treatment but monitoring is also very good option.
- When someone has been diagnosed with PHPT, and the diagnosis is certain, do they need to avoid calcium in their diet? No. The elevated calcium level in the blood stream is decided by the parathyroid tumor not the amount of calcium they have in their diet. It is thought that if the person limits the calcium intake then more calcium will have come out of the bone to go into the blood stream. There have been no studies to see the effect of calcium supplements in the setting of PHPT.
- Can Vitamin D supplementation make PHPT worse? Possibly, in cases when the calcium is very high (for example calcium of 11.5 mg/dl or higher). However, in most other cases it has been shown that vitamin D replacement is safe, can bring the PTH down a little, and more importantly either improve bone density or decrease the rate of bone loss before surgery.